Post by Mikael Svensson, Consultant and Strategic Advisor NHTA
A recent review article published in the European Journal of Health Economics examines NICE’s appraisals of non-small cell lung cancer (NSCLC) models from 2012 to 2022.
There is substantial unmet need in the NSCLC context. For example, in Sweden there are about 4,200 new incident cases of lung cancer diagnosed each year, with a 10-year survival rate of about 20%. While this rate has increased over time, it remains substantially lower compared to other most prevalent cancers, such as breast (>90%) and prostate (around 85%) cancer.
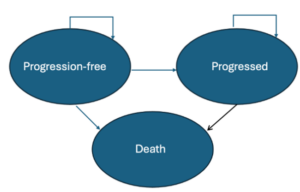
Nonetheless, the drug pipeline in lung cancer care has not been insignificant. The review paper “Trends in NICE technology appraisals of non-small cell lung cancer drugs over the last decade” by Lotte Westerink et al. identified 30 appraisals by NICE in the NSCLC space in the last decade. Of these, 24 were recommended for NHS by NICE and an additional 3 approved via the Cancer Drugs Fund pathway. The typical NSCLC model submitted to NICE nowadays is a Partitioned Survival Model (PSM) with 3 health states and treatment effect assumptions based on an indirect comparison.
In more detail, while Markov cohort models are still the “workhorse” model in most decision model CEA applications, the review showed that PSMs (PSM) is the most common modeling approach in NICE submissions for NSCLC, as they were used in 19 out of the 30 appraisals. Cycle lengths varied between 7 to 30 days, and most models used what can be defined as a lifetime horizon (between 20-40 years).
In line with the trend in most other cancer indications, most models relied on indirect comparisons (performed in 22 out of 30 appraisals), due to lack of appropriate comparators in the pivotal trials. In recent years, the indirect comparisons were mostly based on network meta-analyses or matching-adjusted indirect comparisons (as opposed to mixed treatment comparisons and indirect analysis, which were commonly seen up until 2016).
Many cancer CEA models are becoming increasingly complex given the lack of RCTs with the appropriate comparator and the use of surrogate outcomes as the basis for evaluation. This increasing complexity emphasizes the continued need for advanced HEOR work going forward.